Daliri DB, Laari TT, Ayine AA, Dei-Asamoa R, Volematome BG, Bogee G, et al. Psychosocial experiences of mothers of preterm babies admitted to the neonatal intensive care unit of the Upper East Regional Hospital, Bolgatanga: a descriptive phenomenological study. BMJ Open. 2024;14:e086277.
Google Scholar
Hall SL, Cross J, Selix NW, Patterson C, Segre L, Chuffo-Siewert R, et al. Recommendations for enhancing psychosocial support of NICU parents through staff education and support. J Perinatol. 2015;35:S29–36.
Google Scholar
Hendy A, El-Sayed S, Bakry S, Mohammed SM, Mohamed H, Abdelkawy A, et al. The stress levels of premature infants’ parents and related factors in NICU. SAGE Open Nurs. 2024;10:23779608241231172.
Google Scholar
Malouf R, Harrison S, Burton HAL, Gale C, Stein A, Franck LS, et al. Prevalence of anxiety and post-traumatic stress (PTS) among the parents of babies admitted to neonatal units: A systematic review and meta-analysis. EClinicalMedicine. 2022;43:101233.
Dykes C, Hellman C, Funkquist E-L, Bramhagen A-C. Parents experience a sense of guilt when their newborn is diagnosed small for gestational age, SGA. A grounded theory study in Sweden. J Pediatr Nurs. 2022;62:e8–15.
Google Scholar
Siva N, Velayudhan B, Nayak BS, Lewis LES, Iqbal F, Noronha JA. Interventional Strategies to Mitigate Maternal Stress and Enhance Coping Skills During Neonatal Admission Into Intensive Care Units in Low-and Middle-Income Countries: A Scoping Review. Nurs Open. 2024;11:e70071.
Google Scholar
Deshwali A, Dadhwal V, Vanamail P, Sagar R, Sharma A, Agarwal R, et al. Prevalence of mental health problems in mothers of preterm infants admitted to NICU: A cross-sectional study. Int J Gynaecol Obstet organ Int Fed Gynaecol Obstet. 2023;160:1012–9.
Google Scholar
Grunberg VA, Geller PA, Hoffman C, Njoroge W, Ahmed A, Patterson CA. Parental mental health screening in the NICU: a psychosocial team initiative. J Perinatol. 2022;42:401–9.
Google Scholar
Wang L-L, Meng H-H, Ma J-J, Zhou J. Experiencias de las madres en cuidados intensivos neonatales: una revisión sistemática e implicaciones para la práctica clínica. World J Clin Cases. 2021;9:7072.
Caldwell J, Meredith P, Whittingham K, Ziviani J. Shame and guilt in the postnatal period: a systematic review. J Reprod Infant Psychol. 2021;39:67–85.
Google Scholar
Obeidat HM, Bond EA, Callister LC. The parental experience of having an infant in the newborn intensive care unit. J Perinat Educ. 2009;18:23–29.
Google Scholar
Thivierge E, Luu TM, Bourque CJ, Duquette LA, Pearce R, Jaworski M, et al. Guilt and Regret Experienced by Parents of Children Born Extremely Preterm. J Pediatr. 2023;257:113268.
Google Scholar
Freud S. The Ego and the Id. Vienna: Internationaler Psycho- analytischer Verlag; 1923:1–65.
Bowlby J. Attachment and loss: retrospect and prospect. Am J Orthopsychiatry. 1982;52:664–78.
Google Scholar
Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215.
Google Scholar
Rihan SH, Mohamadeen LM, Zayadneh SA, Hilal FM, Rashid HA, Azzam NM, et al. Parents’ experience of having an infant in the neonatal intensive care unit: a qualitative study. Cureus. 2021;13:e16747.
Google Scholar
Ionio C, Mascheroni E, Colombo C, Castoldi F, Lista G. Stress and feelings in mothers and fathers in NICU: Identifying risk factors for early interventions. Prim Health Care Res Dev. 2019;20:e81.
Google Scholar
Ahmadpour P, Faroughi F, Mirghafourvand M. The relationship of childbirth experience with postpartum depression and anxiety: a cross-sectional study. BMC Psychol. 2023;11:1–9.
Google Scholar
Green G, Tesler R, Marques A. Primiparous and Multiparous Women’s Mode of Birth and Negative Emotions. Int J Environ Res Public Health. 2022;19:1–9.
Google Scholar
Shakarami A, Mirghafourvand M, Abdolalipour S, Jafarabadi MA, Iravani M. Comparison of fear, anxiety and self-efficacy of childbirth among primiparous and multiparous women. BMC Pregnancy Childbirth. 2021;21:1–9.
Google Scholar
Edis EK. The process of becoming a mother from the eyes of primiparous women who had a cesarean section: Qualitative study. Mersin Univ J Heal Sci. 2023;16:65–74.
Yildiz PD, Ayers S, Phillips L. The prevalence of posttraumatic stress disorder in pregnancy and after birth: A systematic review and meta-analysis. J Affect Disord. 2017;208:634–45.
Google Scholar
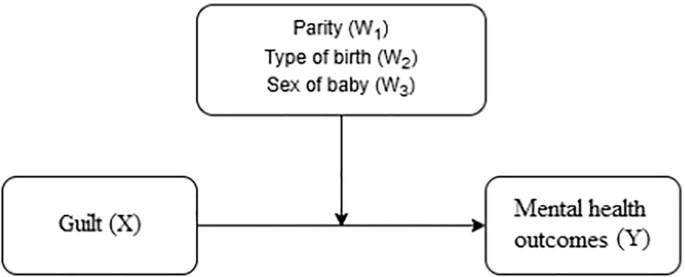
Hayes A. Introduction to Mediation, Moderation, and Conditional Process Analysis A Regression-Based Approach. New York: Guilford Publications, Inc.; 2013.
Hayes A, Montoya A, Rockwood N. The analysis of mechanisms and their contingencies: PROCESS versus structural equation modeling. Australas Mark J. 2017;25:76–81.
Google Scholar
Adama EA, Adua E, Bayes S, Mörelius E. Support needs of parents in neonatal intensive care unit: An integrative review. J Clin Nurs. 2022;31:532–47.
Google Scholar
Caporali C, Pisoni C, Gasparini L, Ballante E, Zecca M, Orcesi S, et al. A global perspective on parental stress in the neonatal intensive care unit: a meta-analytic study. J Perinatol. 2020;40:1739–52.
Google Scholar
Gezer E, Taştekin Ouyaba A. Development of the Guilt Sense Scale in Mothers with Hospitalized Children and Its Psychometric Properties. J Hacet Univ Fac Nurs. 2022;9:240–6.
Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33:335–43.
Google Scholar
Sariçam H. The Psychometric Properties of Turkish Version of Depression Anxiety Stress Scale-21 (DASS-21) in Health Control and Clinical Samples. J Cogn Behav Psychother Res. 2018;7:19–30.
Osborne AD, Yasova Barbeau D, Gladdis T, Hansen K, Branche T, Miller ER, et al. Understanding and addressing mental health challenges of families admitted to the neonatal intensive care unit. J Perinatol. 2025;45:873–80.
Jackson L, O’Donoghue E, Helm J, Gentilcore R, Hussain A. Some Days Are Not a Good Day to Be a Mum’: Exploring Lived Experiences of Guilt and Shame in the Early Postpartum Period. Eur J Investig Heal Psychol Educ. 2024;14:3019–38.
Nomaguchi K, Milkie MA. Parenthood and Well-Being: A Decade in Review. J Marriage Fam. 2020;82:198.
Google Scholar
Park GA, Lee ON. The moderating effect of social support on parental stress and depression in mothers of children with disabilities. Occup Ther Int. 2022;2022:1–8.
Google Scholar
Sánchez-Rodríguez R, Orsini É, Laflaquière E, Callahan S, Séjourné N. Depression, anxiety, and guilt in mothers with burnout of preschool and school-aged children: Insight from a cluster analysis. J Affect Disord. 2019;259:244–50.
Google Scholar
Bozkır B, Çığ O. Examining the Relationship Between Maternal Employment Guilt and Internalized Sexism in Mothers with Preschool Children. Cukurova Univ Fac Educ J. 2022;51:1721–38.
Google Scholar
Kahalon R, Preis H, Benyamini Y. Mother-infant contact after birth can reduce postpartum post-traumatic stress symptoms through a reduction in birth-related fear and guilt. J Psychosom Res. 2022;154:110716.
Google Scholar
Grisbrook MA, Dewey D, Cuthbert C, McDonald S, Ntanda H, Giesbrecht GF, et al. Associations among caesarean section birth, post-traumatic stress, and postpartum depression symptoms. Int J Environ Res Public Health. 2022;19:4900.
Google Scholar
WHO. WHO Statement on Caesarean Section Rates. 2021. https://www.who.int/news-room/questions-and-answers/item/who-statement-on-caesarean-section-rates-frequently-asked-questions.
Khsim IEF, Rodríguez MM, Riquelme Gallego B, Caparros-Gonzalez RA, Amezcua-Prieto C. Risk Factors for Post-Traumatic Stress Disorder after Childbirth: A Systematic Review. Diagnostics. 2022;12:2598.
Google Scholar
Orovou E, Eskitzis P, Mrvoljak-Theodoropoulou I, Tzitiridou-Hatzopoulou M, Dagla M, Arampatzi C, et al. The relation between neonatal intensive care units and postpartum post-traumatic stress disorder after cesarean section. Healthcare. 2023;11:1877.
Google Scholar
Türkoğlu, Balcı NS, Yapalak AN, Acar C, Özyıldırım B. Psychosocial factors in the development of postpartum depression; a case control study. Hippocrates Med J. 2022;2:14–23.
Kahveci G, Kahveci B, Aslanhan H, Bucaktepe PGE. Evaluation of Prevalence and Risk Factors for Postpartum Depression Using the Edinburgh Postpartum Depression Scale: A Cross-Sectional Analytic Study. Gynecol Obstet Reprod Med. 2021;27:227–33.
link